Maternity Care Deserts
A county qualifies as a maternity care desert if it has no hospitals providing obstetric care, no birth centers, no OB/GYN and no certified nurse midwives.
Maternity Care Deserts
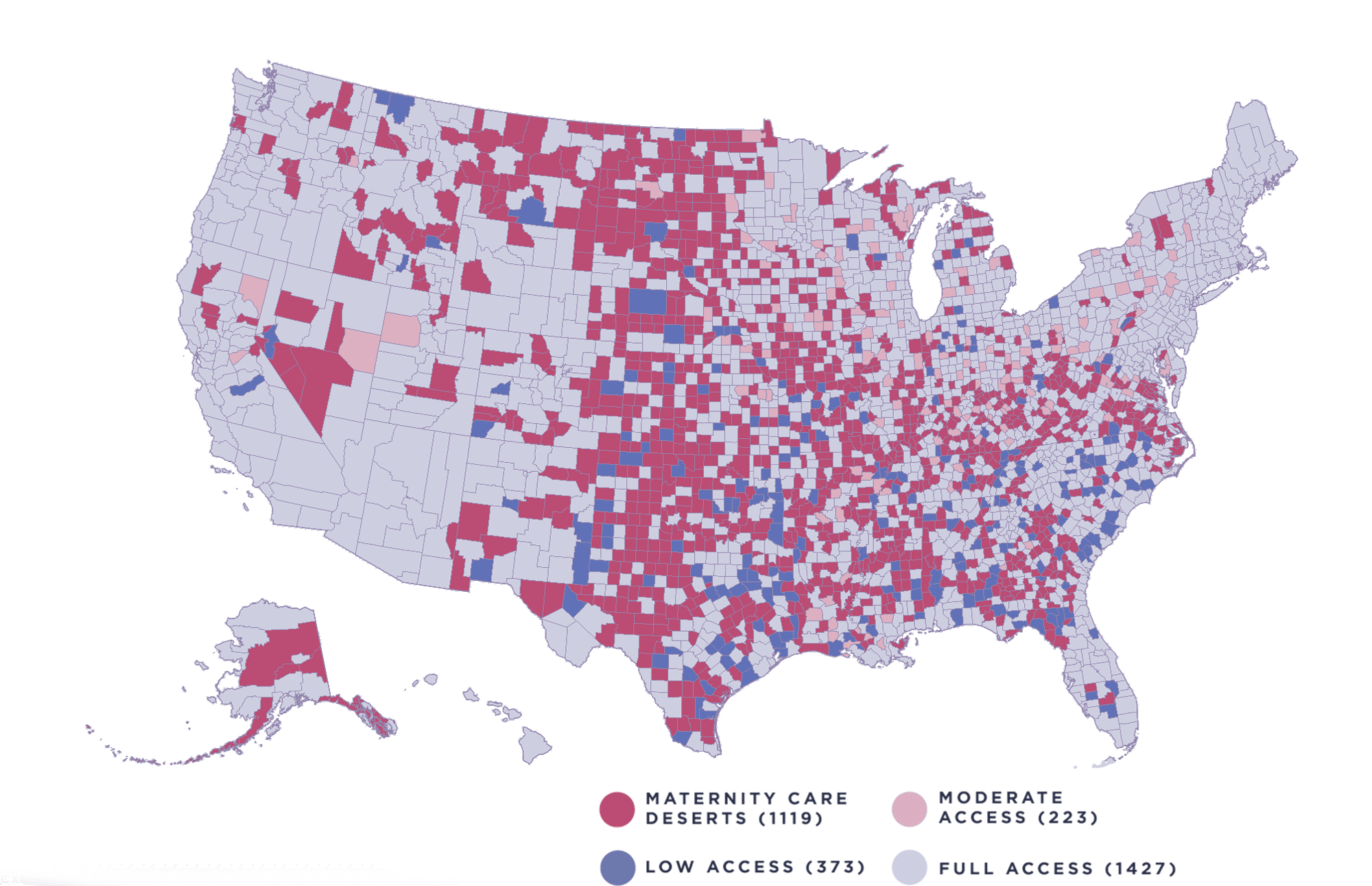
2.3 million women
In 35% of U.S. counties have zero access to maternity care
10% of counties
Have limited access to maternity care
2 in 3
Maternity care deserts are in rural counties
1 in 6
Black infants are born in areas with limited or no access to maternity care
217
Maternity wards have closed across the U.S since 2011
29%
Of rural hospitals nationwide are either at immediate or high risk of closure
Maternity Care Desert Research
A large percentage of women living in areas with limited or no access to maternity care already face a greater share of risk due to social determinants of health; such as limited insurance coverage, food or job insecurity, financial stress, and other challenges.
The issues created by lack of access disproportionately affect low-income women, women of color, and those who live in marginalized communities. Babyscripts addresses geographic and SDOH barriers through our asynchronous tech solution.
Connected health interventions for low-risk pregnant women in a rural population via Babyscripts resulted in healthcare engagement and remote BP monitoring comparable to that observed in the urban setting.
Care coordination facilitated through Babyscripts improved attendance at prenatal care visits and provided a reliable and efficient system that was successfully implemented within an underserved, urban obstetrical population.
Virtual Care Resource Center
Is There a Solution for Maternity Care Deserts?
For a long time, the nation has been putting band-aids on the problem of maternity care deserts, propping up the existing system with temporary fixes, but the problem shows no sign of resolving. And it won't resolve until we recognize that the issues at its heart are not temporary aberrations but reflective of a deeper sea change. We need permanent solutions to meet demographic changes.
Labor Shortages Are Widening Maternity Care Deserts
Pregnant and postpartum women in rural zipcodes are bearing the brunt of recent hospital staffing shortages, as maternity services across the U.S. are being suspended or permanently closed due to lack of resources and dwindling birth rates. Those women are being forced to drive even further distances to access routine care, with the result being that many fail to receive any care at all. Using technology and remote patient monitoring to supplement in-person care can provide a safety net.
The Truth About Maternity Care Deserts
Barriers of access to maternity care are deeply rooted in social determinants of health: problems stemming from income and racial inequality that transcend the urban/rural divide. In the U.S., healthcare has been traditionally considered a triage machine — a last ditch solution when a patient is on the brink of disaster. Solving the issue of maternity care deserts means transforming that outdated mindset.
Innovation, Advocacy, and Maternal Care: Bringing New Life to DC's Maternal Care Desert
Fifty percent of U.S. counties don’t have a practicing obstetrician. That’s an obvious problem. What’s less obvious is that issues of access are not limited to geographic distance but are often rooted in social determinants of health. Dr. Kathryn Marko from George Washington Medical Faculty Associates shares her insights on the state of access and how her DC-based health system has used Babyscripts to bridge the gap.
There is no quick solution for maternity ward closures.
But there are immediate opportunities to improve the circumstances and enhance the chances of safe and healthy deliveries for women in these underserved regions.
The primary concern for these women is not the process of childbirth itself, but the potential for emergency complications. When easy access to an obstetrician is lost, women may opt to forgo prenatal care, which can significantly contribute to pregnancy-related emergencies.
Through Babyscripts, providers at the hospital of delivery or their affiliate practices can offer convenient and accessible prenatal care education to support mothers in the steps toward a healthy pregnancy and educate them on potential warning signs and symptoms.
With remote patient monitoring through Babyscripts, they can anticipate, identify and manage potentially life-threatening complications before they become emergencies, directing expecting mothers to their affiliate practices or to their own maternity ward depending on the necessary care response.
Join our mission of Better Pregnancies.
Want to learn more about how Babyscripts uses remote patient monitoring to improve maternal health outcomes related to maternity care deserts?


-2.png)


