Patient Health Equity
Deidre's Story
A single mother of three, Deidre entered her 3rd pregnancy with chronic hypertension. Her providers enrolled her onto Babyscripts, a decision that she credits with saving her life. Her experience tells a larger story about the barriers of access to maternal health, and the necessary solutions to deliver better outcomes to underserved women. Hear her story in her own words, and learn why she's still making use of her BP cuff.
Health Equity
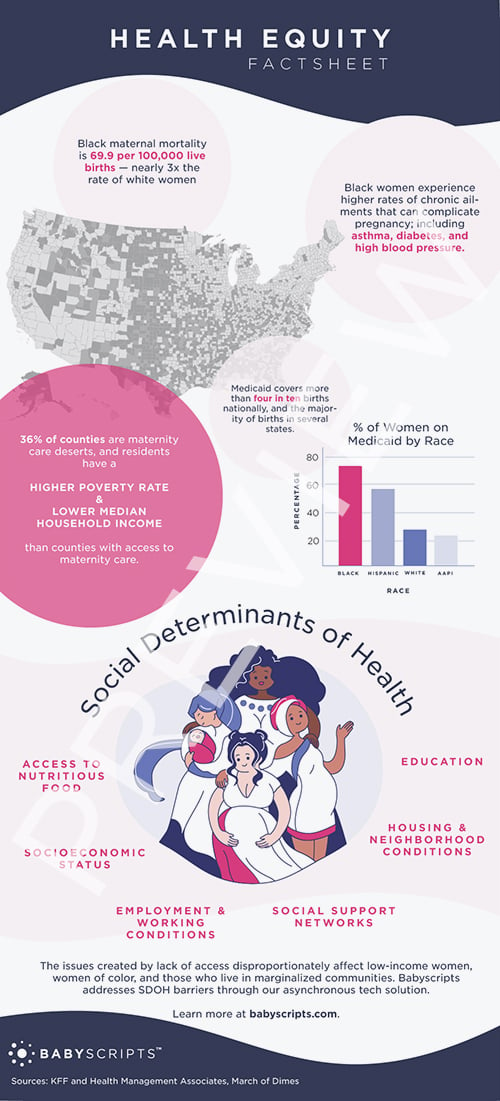
4 in 10
Births covered by Medicaid nationally
3x
Black maternal mortality is nearly 3x the rate of white women
2x
Percentage of Black and Hispanic women on Medicaid, compared to White and AAPI women
Maternal Mortality

Addressing social determinants of health risks is a priority for stakeholders trying to offer a whole-person solution to poor maternal outcomes.
To support these initiatives, the Center for Medicare and Medicaid Services (CMS) has implemented measures that will require hospitals to report data on the screening of patients for certain health-related social needs.
The Screening for Social Drivers of Health measure assesses the proportion of patients screened for the following five social drivers of health: food insecurity; housing instability; transportation needs; difficulty with utilities; and interpersonal safety.
Hospitals will report the total number of patients screened for this information. The related Screen Positive Rate for Social Drivers of Health measure will require hospitals to report the total number of screened patients who indicate that they have one or more of these health-related social needs.
The reporting of 2023 data will be voluntary, and then annual reporting will become mandatory starting with 2024 data.
What is a “social determinant of health” and how can they affect maternal health outcomes?
SDOH include but are not limited to:
Socioeconomic Status
Low income and poverty can contribute to stress and lack of resources like nutritious food and adequate housing
Education
Limited access to education can affect health literacy and the ability to make informed health-related decisions
Access to nutritious food
Limited access to affordable, nutritious food options (food deserts) can contribute to poor nutrition and increase the risk of poor health outcomes
Employment and working conditions
Unemployment, underemployment, and unsafe working conditions can contribute to stress, mental health issues, and lack of access to healthcare services or time off to attend healthcare appointments
Housing and neighborhood conditions
Poor housing quality, overcrowding, and living in neighborhoods with limited access to parks and healthcare facilities can lead to increased exposure to environmental hazards and stressors
Social support networks
Lack of social support systems, including family, friends, and community networks, can impact mental health and overall well-being, and complicate a mother’s ability to attend healthcare appointments as well as focus on her own health after childbirth
Health Equity Research
A large percentage of women living in areas with limited or no access to maternity care already face a greater share of risk due to social determinants of health; such as limited insurance coverage, food or job insecurity, financial stress, and other challenges.
The issues created by lack of access disproportionately affect low-income women, women of color, and those who live in marginalized communities. Babyscripts addresses geographic and SDOH barriers through our asynchronous tech solution.
Use of Babyscripts for low-risk pregnant women in a rural population resulted in healthcare engagement and adherence to remote BP monitoring comparable to that observed in the urban setting, highlighting the opportunity for connected health to reduce health disparities for remote and rural communities.
Care coordination enabled through Babyscripts resulted in improved attendance at prenatal care visits, providing a reliable and efficient system that was successfully implemented within an underserved, urban obstetrical population.
Virtual Care Resource Center
Keeping Patients Safe During Labor Shortages
Labor shortages have left care providers less accessible than ever before, disproportionately affecting socially at-risk women. Babyscripts empowers women with accurate resources, enables them to track vital data and be educated on what that data means, and offers them the security of knowing that their provider will be available to them and intervene in the event of an emergency.
Remote Patient Monitoring to Align with ACOG Guidance, Reduce Health Inequity and Improve Maternal Health
Digital health tools offer women more options for their care, while enabling providers to align with industry recommendations for capturing vital health data regardless of a patient's access to in-person care. In one study, results showed that a much greater percentage of mothers were able to adhere to at-home BP monitoring than the 60% of patients who returned to the office for an in-person BP check.
Health Equity in Obstetrics: Digital Health for Diverse Populations
Technology can extend precision quality care to some of the most vulnerable populations, bridging racial and income disparities through accessible tools that provide objective, data-driven solutions.
To Win Medicaid Contracts, Health Plans Should Prioritize Equity in Maternal Healthcare
With maternal health outcomes worsening across the U.S., state Medicaid plans are hyper-focused on strategies to support pregnancy and postpartum care. Payers should have a plan to adapt current offerings to address the urgent needs of maternity populations.
Join our mission of Better Pregnancies.
Want to learn more about how Babyscripts uses remote patient monitoring to improve maternal health outcomes related to health equity?




