
The use of digital health technology skyrocketed during the pandemic, and the term “telehealth” followed the same trajectory, becoming a buzzword in the healthcare industry and the larger tech community over the past year.
But what does “telehealth” really mean?
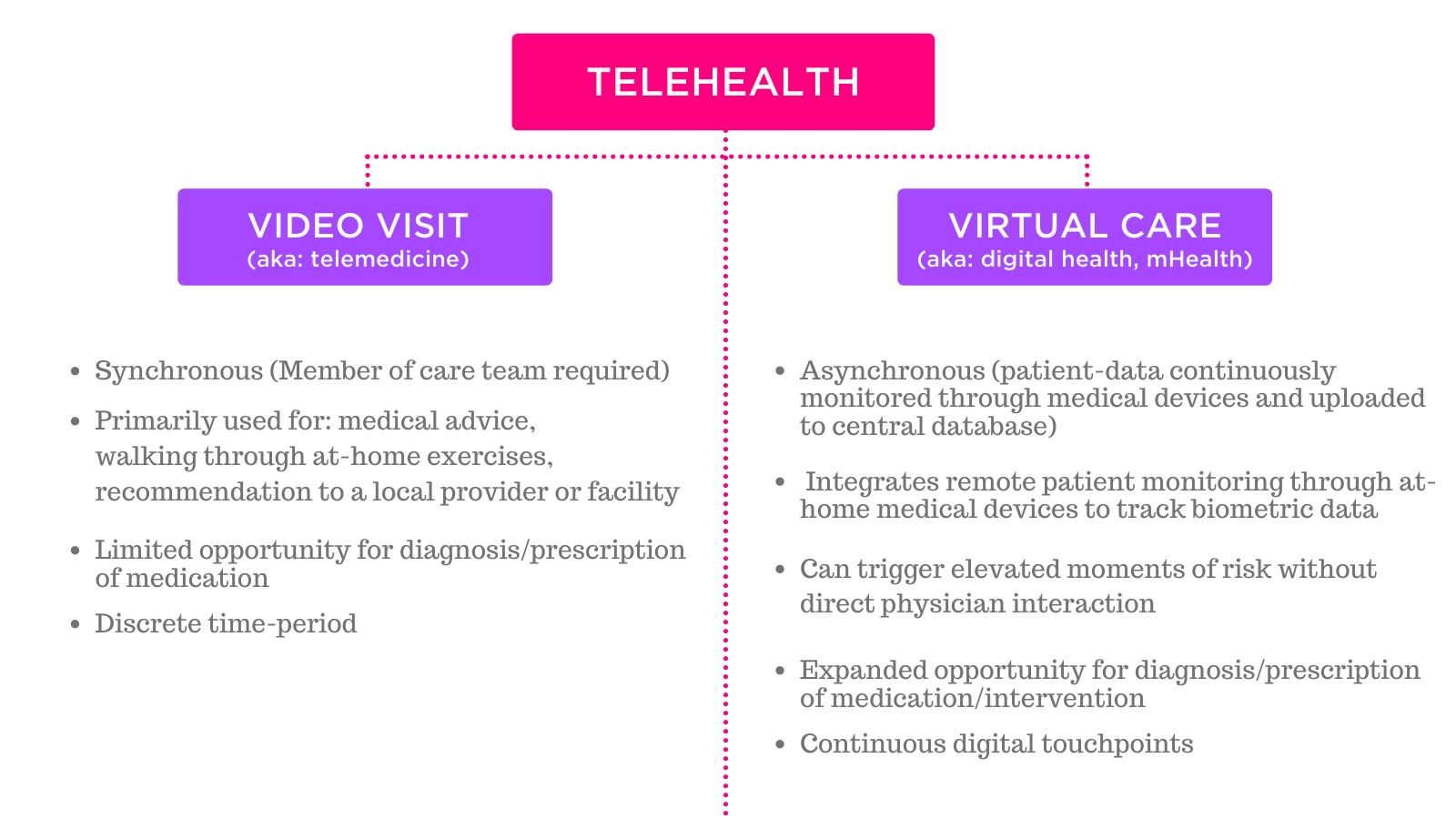
The term has become equivalent to “video visit” — and many health systems will say they offer telehealth when in fact they simply offer synchronous video visits to replace in-person office appointments.
In reality, telehealth is much more comprehensive.
According to the recent ACOG report, Implementing Telehealth in Practice (Jan 2020):
The term “telehealth” refers to the technology-enhanced health care framework that includes services such as virtual visits, remote patient monitoring, and mobile health care.
Video visits are in fact only one small part of telehealth, and one of the least effective in terms of expanding physician reach and improving outcomes. The primary benefit of a video visit is convenience, and comfort or safety for those anxious to return to public places in wake of the pandemic.
While some clinical diagnoses are possible through a video visit, the list is limited without access to biometric data or an in-person exam. As a physician is required to be on the other side of the exchange, video visits do nothing to address the problems of the physician shortage, although they can improve access for patient populations.
According to a review from George Washington University on the specific benefits of telehealth for obstetrics (with a scope that includes low-risk and high-risk obstetrics, family planning, and general gynecology), the potential benefits in telehealth interventions rest particularly in text-based and remote monitoring.
Virtual care, also termed “digital health” or “mHealth,” refers to this concept of mobile self-care or remote patient monitoring. While virtual care can and often does incorporate video visits, it is much more comprehensive.
Virtual care (like we provide at Babyscripts) works via consumer technologies like smartphone and tablet apps, with at-home medical devices like blood pressure cuffs, weight scales, and glucometers. These medical device can either be “connected,” which means the device has a bluetooth or cellular chip inside that allows the device to automatically connect to the cloud after a reading is taken; or a device can be “manual,” which means that after a reading is taken, the patient manually uploads that value into a portal or interface to connect the data to a central database (aka the EMR).
Virtual care enables patients to capture their own health data, enabling asynchronous modalities of monitoring and managing patients, and directly addressing the issues of the physician shortage, access to care, and outcomes.
For more info, read Virtual Maternity Care: A Complete Playbook, an implementation guide and compilation of best practices and resources for transforming your practice through technology; and Medicaid Playbook: Part I, a guide for delivering digital tools to Medicaid populations.

Submit a comment