In these times of uncertainty and ever-evolving policies and practices, Babyscripts is committed to sharing the benefit of our long experience in the field of innovation, specifically virtual maternity care. We’re keeping our clients and others abreast of the latest in clinical guidance, best practices, market intelligence, and other topics through our virtual care resource center (subscribe here) as well as through a webinar series with some of our large health system partners (register for our June 24 webinar with Dr. Mark B. Woodland of Tower Health System).
Most recently, we sat down with George Washington Medical Faculty Associates (GW-MFA) OB-GYN leadership and providers — longtime partners of Babyscripts and forerunners in the digital health field — to discuss their approach to research and innovation in women's services, and how this approach has helped them respond to COVID-19.
Panelists included:
Nancy Gaba, MD, FACOG, Oscar I. and Mildred S. Dodek and Joan B. and Oscar I. Dodek, Jr. Professor and Chair, Department of Obstetrics and Gynecology
Kathryn Marko, MD, FACOG, NCMP, Assistant Professor of Obstetrics and Gynecology and Residency Program Director
Anna BuAbbud, MD, Assistant Professor of Obstetrics & Gynecology
Kaitlyn Molé, CNM SANE-A PMH-C, Clinical Instructor
Read the recap below:
Commitment to Health Equity
The scheduled subject of discussion for this webinar was the crisis of COVID-19 and its impact on women’s reproductive health — but as Dr. Gaba highlighted in her introduction, there is a crisis of hatred and discrimination rampant in our country right now that must also be addressed.
In the conversation around innovation in women’s services, the imperative lies on all participants to make sure that innovative solutions are equitable and available to all women regardless of race or income level.
History of Innovation at GW-MFA
GW-MFA has been a research partner of Babyscripts since its inception, helping its bachelor founders figure out the critical components of prenatal care. Working together, they considered how technology could supplement prenatal care to make it more robust, and also how to reimagine prenatal care and make the ideal form a reality.
What GW-MFA has done with Babyscripts is look critically at what the platform does for patients, as well track patient responses to the program.
They’ve found that
- Babyscripts increases patient satisfaction and connection
- Patients appreciate resources and education from trusted sources like ACOG and the CDC
- Remote care allows providers to schedule appointments at critical times, giving patients more time in their busy schedules
GW-MFA has been able to reduce in-person visits without any negative outcomes, using remote monitoring of blood pressure to collect more data and follow patients more closely than possible with an in-office blood pressure check and point of care solution. This rethinking and right-sizing of prenatal care has been more important than ever in recent times, as COVID-19 has forced practices to transition care out of the office.
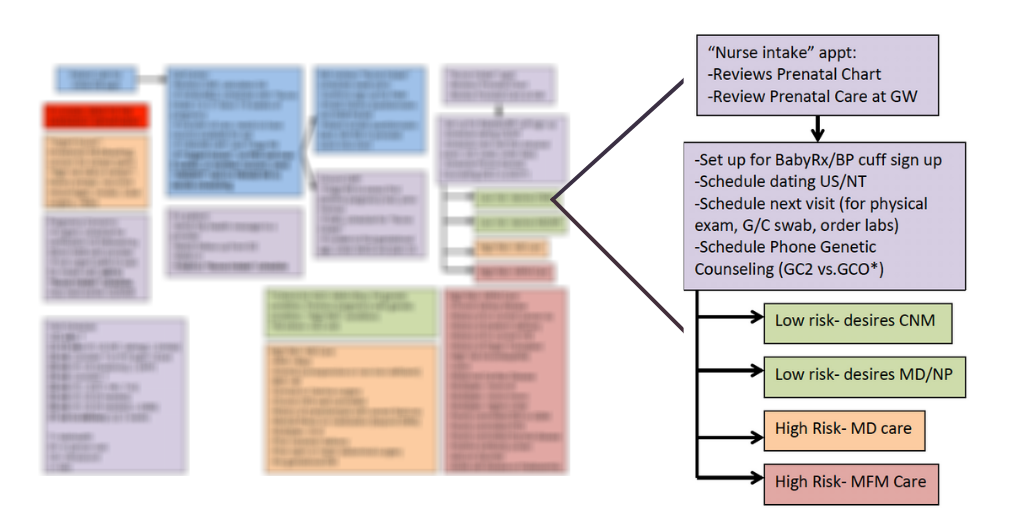
For access to all webinar slides, including workflow, view the webinar here.
With a database of >80,000 pregnancies (including >120,000 blood pressure data points and >30,000 weight measurements), GW-MFA has been able to critically examine outcomes and determine the benefits of the program for those that have gone through it. They’ve used this wealth of data to look closely at the interventions that are available/possible, and the critical timing of those interventions, leveraging it in a move toward precision medicine and ultimate reduction in health disparities in rural communities and DC.
UPCOMING: Register here for our webinar with Mark B. Woodland, MS, MD, FACOG, Chair, OB-GYN Reading Hospital/Tower Health System on JUNE 24, 10AM
DC’s Maternity Care Desert
GW-MFA serves patients from the larger DMV area (DC, Maryland, and Virginia), but the greatest disparities in maternity care are found in their home city of Washington, DC. DC has some of the highest rates of maternal mortality in the US — higher even than some third world countries — with a particularly high incidence of preterm births.
Rates of preterm birth are highest in Wards 7 and 8, east of the Anacostia river and home to some of the poorest and most health-needy citizens in the city. The rate of infant mortality in these wards is second only to the adjacent Ward 5. The crisis is due primarily to the closure of two hospitals that delivered OB care — women who are seeking care now have to travel across the city to access it, sometimes taking two or three methods of transportation and spending a half day to attend a ten-minute, routine appointment. Taking that time out of the day is difficult for anyone, but especially for women who struggle with barriers of transportation, childcare, and hourly jobs that don’t offer leave.
Babyscripts recognized the need for creative solutions for these health-challenged populations, and created a model in which payers could subsidize the cost of their virtual maternity solution for patients. As a result of that forward-thinking, GW-MFA now partners with Amerigroup and Amerihealth, two of the largest MCOs in DC, to help connect patients facing barriers to access with prenatal care. These types of partnerships between innovators, healthcare providers, and payers represents one of the biggest strides toward solving the healthcare crisis.
Response to COVID-19
When the pandemic hit, GW-MFA found themselves in the same position as health systems across the country — needing to quickly decide how to streamline the process of patient care to minimize in-person visits but optimize access for all patients.
They used the model of Babyscripts Schedule Optimization — reducing visits through remote monitoring and a trigger alert system — to think about how to most appropriately provide care. Prior to COVID-19, GW-MFA had some exclusion criteria for patients using Babyscripts, but the pandemic drove the need to standardize entry into the practice and use Babyscripts for all patients.
Through Babyscripts, the practice is able to provide to-the-minute resources on things like policy changes and symptom information, as well as resources specifically targeted to the social challenges of the stay-at-home order, like food insecurity and domestic violence.
Prior to the pandemic, patients saw one provider — now patients see multiple providers, but they have a standard set of resources from Babyscripts. These resources and week-to-week data have empowered patients and enhanced their care, and knowing that providers are monitoring for outliers makes them feel secure.
Patient Empowerment through the Pandemic
Most providers can speak to increased anxiety in their patients, especially during pregnancy and postpartum — and the pandemic only serves to increase this anxiety.
GW-MFA used Babyscripts to distribute documents for COVID-19 and mental health-related options, such as nutrition, intentional body movement, and hotline information. They also worked on streamlining telehealth visits, sending out virtual mental health surveys beforehand through the Babyscripts app, which increased completion rates and improved the visit itself.
These digital avenues for care such as telehealth visits and the Babyscripts app have changed the dynamic of patient visits. Patients may feel more open and connected with their providers when they are in the comfort of their home, receiving care through the power neutral setting of a video visit.
The Impact of Babyscripts: A Patient Case Study
One of the most important benefits that GW-MFA has experienced through Babyscripts is identification of high risk conditions at significantly earlier times than typically identified.
One 35-year-old patient, enrolled on Babyscripts at 7 weeks gestations, had 26 blood pressure data points recorded. She followed an optimized schedule for her prenatal care visits, attending 8 standard appointments, and had a repeat C-section. On postpartum day 4, she was noted to have increased swelling and elevated blood pressure. With the elevated blood pressure, a trigger alert was sent through the Babyscripts cloud to the GW-MFA triage center. The patient was instructed to return to the hospital, ultimately diagnosed with preeclampsia with severe features, and received postpartum magnesium for 24 hours and hypertension medication. She was discharged and her providers were able to titrate her blood pressure medication remotely through telehealth and Babyscripts. At 11 weeks postpartum, the patient was normotensive, and her providers were able to wean her off of hypertension medication.
This is one of several similar case studies that the physicians at GW-MFA have collected through their research.
The Impact of COVID-19 on Practice
While it’s too soon to say much about the financial impact of COVID-19, it is clear that all health systems are impacted by the economic fallout. At GW-MFA, the practice is particularly struggling to ensure that all patients have access to care.
Ensuring that patients don’t put off their healthcare because of the pandemic is the top priority. Following closely on the heels of that is the assurance that the practice be paid for the services they are providing to patients. As GW-MFA is optimizing care and converting to a mix of virtual and in-person care, they’ve analyzed how they are being reimbursed.
Like all health systems, GW-MFA is struggling with understanding the ever-evolving rules for coding and billing for these services. For most patients, they are billing with global codes, which has not represented a significant change. For patients that are billed individually, they have up to this point been reimbursed for virtual visits appropriately.
With COVID-19 limiting in-office appointments, the need to enhance access to care with virtual solutions like Babyscripts was essential. Being able to optimize OB visits and deliver some of that care from home has enabled GW-MFA to allocate care and see more urgent cases in-office.
The Future of Obstetric Care
On the future of OB care post-pandemic, both generally and specific to GW and Babyscripts, the panelists had this to say:
“The pandemic has opened my eyes as a leader in women’s health to some of the opportunities that we have — I’m an optimist and I think the future is very bright. Even though the pandemic has been a horrifying crisis for our nation and the world, I think there will be positive outcomes for OB care. Most women who are of childbearing age are used to technology, so the future of OB care means enhancing their experience with apps.” - Dr. Gaba
“We intend to continue to use these tools at GW to keep our patients connected through improved and up-to-date resources, like info on our visitor policy, access to the flu vaccine for our patients, and other time-sensitive topics. We also want to explore group prenatal care. We have grants in the department bookmarked to enhance group prenatal care, and we’re looking forward to using the Babyscripts app to supplement that.” - Dr. Marko
“Using the technology of Babyscripts to identify high risk conditions in pregnancies, at whatever time throughout a woman’s pregnancy, is one of its greatest assets. The app is really helpful for empowering patients to ask the right questions, and introducing them to the ways that they can be more involved in care. It creates a more interactive model of care to help improve access for all.” - Dr. BuAbbud
“Among the midwives, we enjoy telehealth for meeting patients where they’re at — it’s a unique opportunity to remedy some of the health inequity in DC and one that is critical to continue post-pandemic.” - Ms. Molé
Q&A
Why did GW decide to work with an outside vendor instead of building a solution in-house?
It felt more organic than an “outside” company. The founders of Babyscripts were very linked in with the innovators at GW — they approached us to help develop some of the content for the app. It felt like we were at the grassroots level. At the time, we weren’t doing anything remotely like this, but the vision was there, and while it was an outside company, it felt internal in some ways. Because we had a lot of buy-in as the content experts in the department, we were completely sold from the beginning.
The MFA’s mission is not just providing healthcare, it’s providing healthcare in the setting of education and research, and working with the folks here who were originally involved with Babyscripts, we made that very clear — and they supported that from the beginning.
For a practice who has not used tech before, tell us a little bit about the obstacles you had to overcome for implementation?
Buy-in is the biggest obstacle. It was very challenging to get anything new past the “if it’s not broke, don’t fix it” attitude. It took us a while to demonstrate the benefits of the platform to the providers. Now we have made it the default rather than the exception — something that every provider is signed up for. Unfortunately it took the pandemic to get there.
One of the reasons that people were unsure about using the app for their patients was because they didn’t understand that prenatal care could be delivered in a better or different way. Instead of finding the exceptions who could be on Babyscripts — who is the right patient for this — we’ve now put everyone on Babyscripts. Now we consider how we help the outlier patients with additional tools.
We realized that Babyscripts would be the best resource for the most up-to-date info on what was going on, and also for delivering resources that we had actively composed, because everyone has access, everyone has buy-in on the resources that are delivered.
Initially we had exclusion criteria (high risk patients specifically) — we wanted to have more control, more close watch over these patients. Now that we have everyone involved, enrolling all patients regardless of risk, we can check in through telehealth, and they have the option to use remote monitoring as an additional resource.
At the very beginning of the pandemic when we were bracing for the surge and worried about being disconnected from patients, we felt very strongly that getting everyone signed up and with a blood pressure cuff was crucial. We really wanted all of our patients to feel like they had access to us at all times even without in-person visits.
High risk patients have not been excessive versus what we expected in terms of after hours calls and triage center calls, which makes me realize that we were probably being too restrictive before in the limit of patients that we were putting on technology.
People are still coming in for ultrasounds and other prenatal care, and it helps us keep track of high risk patients who need closer monitoring.
Can you comment on ease of use for patients?
Patients love it — it’s extremely easy regardless of bluetooth-connected blood pressure cuff or manual entry. The graphs help the patients easily map their progress (and the 2.0 version is even better).
For providers, there is a portal that is easily searchable. Providers can see patient blood pressure history, and easily titrate or start medication. There is the ability to integrate directly, and although our current EMR does not do so, we are hoping to change that soon.
About GW-MFA
The GW Medical Faculty Associates is the largest independent physician practice in the Washington DC metro region. As members of The GW School of Medicine and Health Sciences faculty, the providers are teachers and mentors for medical students, residents, and researchers preserving a rich tradition of academics, research, and healing.
Register here for our next webinar!
For the latest on clinical guidance, best practices, market intelligence, and more, subscribe to our Virtual Resource Center.

Submit a comment